|
COVID-19 and Dystonia Care: What do you need to know? While we patiently wait for the COVID-19 crisis to resolve, we approached leading dystonia experts for tips and advice on caring for patients. We were fortunate to sit down with one of the leading clinical and research experts, neurologist Dr. Aparna Wagle Shukla. She shared with us her “top 5” tips for dystonia care during the COVID crisis. Who is Dr. Aparna Wagle Shukla?
What should every dystonia patient know about the Corona virus?
THERE IS NO VACCINE FOR COVID AT THE CURRENT TIME WHICH MEANS PREVENTION IS THE KEY.
What are important precautions every dystonia patient should take at home?
How important is social distancing for dystonia patients? What is the risk of COVID-19 in dystonia?
What should a dystonia patients know about medication management during the COVID-19 crisis? What about the need to see a doctor during the COVID crisis?
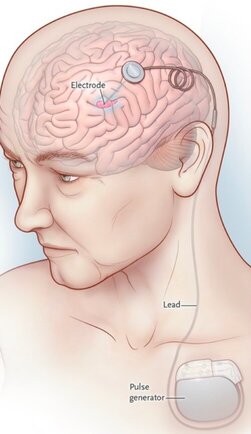
What do you tell dystonia patients with deep brain stimulation (DBS) devices during the COVID-19 outbreak?
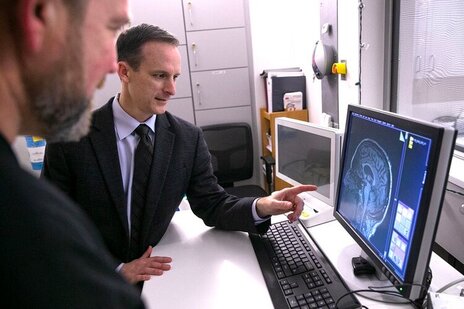
There are so many exciting projects going on in dystonia research that it has become hard to keep up with all of the advances. We sat down with one of the worlds top dystonia and Parkinson imaging researchers (Dr. David Vaillancourt) to talk about the “top 5” updates in therapies and in dystonia imaging research. Who is David Vaillancourt?
1) What is imaging and how is it used in dystonia?
2) What is a specific example in humans for how imaging is being used in dystonia?
3) What is a specific example in animals for how imaging is being used in dystonia?
4) How can imaging be used in humans to assess a new therapeutic (e.g. drug, device)?
5) What does this all mean for people with dystonia?
|
Archives
September 2021
Categories |
Location:
|















 RSS Feed
RSS Feed